
How to improve your emergency department through Lean management
Author: Sandra Rueda Charro
Data: 03.09.2019
Keywords
Lean, Lean management, Lean healthcare, Lean methodology, Emergency department, Lean six sigma.
Have you ever wonder how would your emergency department (ED) look like if you could apply an efficient workflow and eliminate activities that don’t add any value? Lean management is here to help you.
About Lean
Lean healthcare is an attempt to transfer the lean management to healthcare in order to make it more efficient. Lean is a methodology that seeks continuous improvement and elimination of actions and processes that do not add any value for the patient, he/she wouldn’t pay for, that do not help him/her to heal or be more satisfied with the care. Lean healthcare will allow us to reorganize the crowded emergency departments and redirect all the resources which are wrongly used towards a more quick and safer attention to the patients.
Why are emergency departments overcrowded?
The growing overcrowding of European emergency services is a real challenge for governments and health managers. There are several factors that are contributing to this problem, among which are:
Social factors: Mainly, the European population is increasing, as well as the proportion of elder people. This is making chronic diseases more prevalent
Economic factors: European governments are trying to reduce health budget by reducing the workforce and other resources. Health services are expected to do more with less.
Overtreatment: 1 in 10 patients receive a harmful, unnecessary or non-valuable treatment to their health outcomes.
Work organization: (we will focus more on these):
- The work is organized around compartments of the human body instead of being organized around health processes, which results in a fragmented care (with more expenditure).
- There is a poor communication between different professionals or areas.
- After triage (mainly performed by nurses), patient’s diagnosis is usually left in the hands of junior physicians.
- Lack of care standardization. Diagnosis and treatment variability threatens patient safety and increases overall spending.
- When professionals get involved in several tasks at once, the workflow is hindered.
- Mismatch of capacity and demand.
- Inefficient distribution of the different spaces. This produces a lot of unnecessary movements of staff and patients, and should be addressed according to hospital engineering knowledge.
- Poor organization of hospital admissions and discharges.
With Lean healthcare we cannot change economic or social factors, but surely we can act on work organization and standardization of care. This should be a main concern of hospital managers, to ensure the safety of his/her patients, the satisfaction of his employees, and the efficient use of resources.
A pathway to implement lean management successfully
To successfully go Lean, we will take into account the 5 Lean principles (define value, map the value stream, create flow, establish pull, pursue perfection) and adjust them to our own pathway. After the managers have decided to go Lean, they should take a look to the institution culture. It’s important to remove the “culture of blame” and redirect it towards a culture of critical thinking and willingness to solve problems. Also, the staff should be informed and trained on the importance of patient safety.
Define value. As we said before, we need to decide what is value for us. The patient must be the reference according to which we decide what is valuable and what is waste.
Map the value stream. We need to map our current value stream and the ideal one. Thinking about the patient as the protagonist, we have to write down every single step of his/her pathway in our ED, and also the time he/she spends in every step.
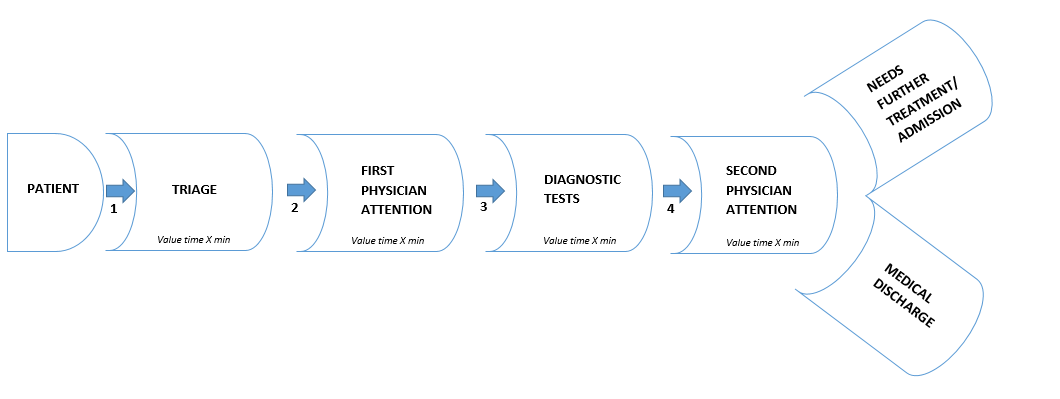
Create flow. Doctors often decide to evaluate new patients instead of discharging the ones that already have their tests done. In order to keep an adequate flow, we should follow FIFO principle “First In First Out”. If a patient can already be discharged, we should go for it immediately. Technology could help with this purpose, by providing tools like a screen where you can see the patient’s status, and the availability of the diagnostic tests performed.
Establish pull. The ED capacity must depend on demand, not on organizational preferences. Takt time can be used on each part of the ED to calculate the staff needs. Also we should make a statistical study about our ED’s patient flow each hour (daily) paying attention to our seasonal flow too. This way we would improve staff shifts to adjust them to demand.
Pursue perfection. This is based on continuous improvement (kaizen). In each work shift we should designate at least a doctor, a nurse, a radiology technician, a laboratory technician and a manager trained in Lean methodology to be able to carry out an adequate workflow. They should meet at least once daily to detect existing problems and solve them. Prior to installing Lean in our ED and from time to time, we should conduct few kaizen events to train our staff in the improvement culture and to teach them how Lean works. A good problem-communication informatic tool could be helpful to our purpose since all the workers can communicate problems they find in the field.
Other tools which can help us (lean or not lean):
Five S:
- Remove anything useless from the workspace.
- Set in order. Organize the workspace effectively.
- Keep the workplace clean.
- Standardize the processes used to sort, order and clean the workplace.
- Keep improving.
New technologies: Telemedicine can help manage chronic patients more efficiently and avoid emergency attendance. Digitalized X-rays and lab results can accelerate lead time. Lastly, a good electronic medical record shared by all health providers can avoid diagnostic tests duplication.
Checklists in critical activities.
Strengthening primary care and appointing case management nurses for the management of chronic processes.
Use of generic drugs.
Multidisciplinary improvement teams to centralize problem solving according to the scientific method.
PDCA cycle: Plan, do, act, check. Continuous improvement is not possible if we don’t evaluate what we do and plan improvements.
Work standardization, use of clinical guidelines. Implement fast tracks with stable work teams for the most serious and frequent pathologies (chest pain, stroke …).
Visual management: Colored paths (they will make easier patient’s journey in our ED)
References
Literature:
[1] Burström, L., Nordberg, M., Ornung, G., Castrén, M., Wiklund, T., Engström, M., Enlund, M. (2012). Physician-led team triage based on lean principles may be superior for efficiency and quality? A comparison of three emergency departments with different triage models. Scandinavian journal of trauma, resuscitation and emergency medicine, [online] Available at: https://sjtrem.biomedcentral.com/articles/10.1186/1757-7241-20-57
[2] Hogan, B., Rasche, C., von Reinersdorff, A. The First View Concept: introduction of industrial flow techniques into emergency medicine organization, 19(3), pp. 136-139.
[3] Burström, L., Letterstål, A., Engström, M., Berglund, A., Enlund, M. (2014). The patient safety culture as perceived by staff at two different emergency departments before and after introducing a flow-oriented working model with team triage and lean principles: a repeated cross-sectional study. BMC health services research, [online] Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4105242/
OECD (2017). Tackling Wasteful Spending on Health. OECD Publishing, Paris.
Abdallah, A. (2014). Implementing quality initiatives in healthcare organizations: drivers and challenges. international Journal of health care quality assurance, 27(3), pp. 166-181.
Balfour, M., Tanner, K., Jurica, P., Llewellyn, D., Williamson, R., Carson, C. Using Lean to Rapidly and Sustainably Transform a Behavioral Health Crisis Program: Impact on Throughput and Safety. Joint Comission Journal on quality and patient safety, 43(6), pp. 275-283.
Banerjee, A., Mbamalu, D., Hinchley, G. (2008). The impact of process re-engineering on patient throughput in emergency departments in the UK. International journal of emergency medicine, 1(3), pp. 189–192.
Bruno, F. (2017). Lean thinking in emergency departments: concepts and tools for quality improvement. Emergency Nurse, 25(6), pp. 38-41.
Bucci, S., De Belvis, A., Marventano, S.,De Leva, A., Tanzariello, M., Specchia, M., Ricciardi, W., Franceschi, F. (2016). Emergency Department crowding and hospital bed shortage: is Lean a smart answer? A systematic review. European Review for Medical and Pharmacological Sciences, 20(20), pp. 4209-4219.
Chan, H., Lo, S., Lee, L., Lo, W., Yu, W., Wu, Y., Ho, S., Yeung, R., Chan, J. (2014). Lean techniques for the improvement of patients’ flow in emergency department. World journal of emergency medicine, 5(1), pp. 24–28.
Decker, W., Stead, L. (2008). Application of lean thinking in health care: a role in emergency departments globally. International Journal of Emergency Medicine, 1(3), pp.161–162.
Dickson, E., Singh, S., Cheung, D., Wyatt, C., Nugent, A. (2009). Application of lean manufacturing techniques in the Emergency Department. Journal of Emergency Medicine, 37(2), pp. 177-182.
Kaplan, G., Patterson, S., Ching, J., Blackmore, C. Why Lean doesn’t work for everyone. BMJ quality & safety, 23(12), pp. 970-973.
Kelly, A., Bryant, M., Cox, L., Jolley, D. (2007). Improving emergency department efficiency by patient streaming to outcomes-based teams. Australian Health Review, 31(1), pp. 16-21.
Mazzocato, P., Savage, C., Brommels, M., Aronsson, H., Thor, J. Lean thinking in healthcare: a realist review of the literature. Quality & Safety in health care, 19(5), pp. 376-382.
Mazzocato, P., Thor, J., Bäckman, U., Brommels, M., Carlsson, J., Jonsson, F., Hagmar, M., Savage, C. (2014). Complexity complicates lean: lessons from seven emergency services. Journal of Health Organization and Management, 28(2), pp. 266-288.
Mousavi Isfahani, H., Tourani, S., Seyedin, H. (2019). Features and Results of Conducted Studies Using a Lean Management Approach in Emergency Department in Hospital: A Systematic Review. Bulletin of Emergency and Trauma, 7(1), pp. 9-20.
Niemeijer, G., Trip, A., Ahaus, K., Does, R., Wendt, K. Quality in trauma care: improving the discharge procedure of patients by means of Lean Six Sigma. The journal of trauma, 69(3), pp. 614-618.
Radnor, Z., Holweg, M., Waring, J. (2012). Lean in healthcare: The unfilled promise?. Social Science & Medicine, 74(3), pp. 364-371.
Ryan, A., Hunter, K., Cunningham, K., Williams, J., O’Shea, H., Rooney, P., Hickey, F. STEPS: lean thinking, theory of constraints and identifying bottlenecks in an emergency department. Irish medical journal, 106(4), pp. 105-107.
Sánchez, M., (2014). Lean healthcare en los servicios de urgencias hospitalarios. ¿Ha venido para quedarse?. Emergencias, 26(1), pp. 81-83.
Sánchez, M., Suárez, M., Asenjo, M., Bragulat, E. (2018). Improvement of emergency department patient flow using lean thinking. International journal foy quality in health care, 30(4), pp. 250-256.
Tejedor-Panchón, F., Montero-Pérez, J., Tejedor-Fernández, M., Jiménez-Murillo, L., Calderón de la Barca-Gázquez, J., Quero-Espinosa, F. (2014). Mejora del proceso de un servicio de urgencias de hospital mediante la metodología Lean. Emergencias, 26(1), pp. 84-93.
Timmons, S., Coffey, F., Vezyridis, P. (2014). Implementing lean methods in the emergency department: the role of professions and professional status. Journal of Health Organization and Management, 28 (2), pp. 214-228.
Morcillo, A. (2013). Implantación de la metodología Lean en un servicio de urgencias. Universitat de Barcelona. Escola Universitària d’Infermeria, Madrid, España.
Websites:
Andersen, H., Røvik, K., Ingebrigtsen, T. (2014). Lean thinking in hospitals: is there a cure for the absence of evidence? A systematic review of reviews. BMJ, [online], Available at: https://bmjopen.bmj.com/content/4/1/e003873 (retrived on 03.09.2019)
Improta, G., Romano, M.,3, Di Cicco, M., Ferraro, A., Borrelli, A., Verdoliva, C., Triassi, M., Cesarelli, M. (2018). Lean thinking to improve emergency department throughput at AORN Cardarelli hospital. BMC Health Services Research, [online] Available at: https://bmchealthservres.biomedcentral.com/articles/10.1186/s12913-018-3654-0 (retrived on 03.09.2019)
Mazzocato, P., Holden R., Brommels, M., Aronsson, H., Bäckman, U., Elg, M., Thor, J. (2012). How does lean work in emergency care? A case study of a lean-inspired intervention at the Astrid Lindgren Children’s hospital, Stockholm, Sweden. BMC Health Services Research, [online] Available at: https://bmchealthservres.biomedcentral.com/articles/10.1186/1472-6963-12-28 (retrived on 03.09.2019)
McCulloch, P., Kreckler, S., New, S., Sheena, Y., Handa, A., Catchpole, K. (2010). Effect of a “Lean” intervention to improve safety processes and outcomes on a surgical emergency unit. BMJ, [online], Available at: https://www.bmj.com/content/341/bmj.c5469 (retrived on 03.09.2019)
Rodrigues Terraa, J., Tobal Berssanetia, F. (2018). Application of lean healthcare in hospital services: a review of the literature (2007 to 2017). Production, [online] Available at: http://www.scielo.br/scielo.php?pid=S0103-65132018000100402&script=sci_arttext (retrived on 03.09.2019)
Vorne Industries Inc (2011-2019). Theory of Constraints. [online] LeanProduction. Available at: https://www.leanproduction.com/theory-of-constraints.html (retrived on 03.09.2019)
Wikipedia.org (2019). Sistema de producción Toyota. [online] available at: https://es.wikipedia.org/wiki/Sistema_de_producci%C3%B3n_Toyota (retrived on 01.09.2019)
Wikipedia.org (2019). 5S (methodology). [online] available at: https://en.wikipedia.org/wiki/5S_(methodology) (retrived on 01.09.2019)
Do, D. (2017). The Five Principles of Lean. [Blog] The Lean way blog. Available at: https://theleanway.net/The-Five-Principles-of-Lean (retrived on 30.08.2019)
http://www.gregoryschmidt.ca/writing/stocking-hospital-supply-rooms-two-bin-kanban(retrived on 30.08.2019)

